Deterioration in a person’s health can manifest in various ways, and its identification is crucial in providing appropriate care. This educational resource aims to highlight the importance of recognising signs of deterioration, why it matters, what healthcare professionals need to know, and the tools and actions they can employ to address it effectively.
5 Key Takeaways of Recognising Acute Deterioration
- Understanding and Recognising why Deterioration Matters
- Indicators of Deterioration
- Role of the Registered Nurse Including Assessing, Responding, and Coordinating
- Communication
- Critical Nurse Interventions
Understanding and Recognising why Deterioration Matters
Understanding Deterioration: Deterioration refers to observable indicators of a person’s declining or reduced state of health. These signs may include increased time spent in bed, reduced food intake, difficulties in swallowing, excessive sleep or rest, and fluctuating consciousness.
Why Recognising Deterioration Matters: Recognising deterioration is vital for several reasons:
- Review of Care Needs and Goals: It allows for a thorough evaluation of care needs and care goals, involving the individual (if possible), their family, and their general practitioner (GP) or Nurse Practitioner (NP).
- Initiating Palliative Care: Identifying deterioration is a key step in initiating a palliative care plan or pathway when appropriate.
- Respecting Wishes: It ensures that care aligns with the individual’s wishes, promoting patient-centered care.
- Symptom Management: Early recognition enables healthcare providers to manage symptoms effectively, enhancing the patient’s quality of life.
- Appropriate Treatment: Recognising deterioration facilitates the withdrawal of treatments, activities, or medications that are no longer beneficial or suitable for the patient.
- Counseling and Support: It allows for the provision of counseling and support to both the patient, their family, and healthcare staff.
- Preventing Unnecessary Hospital Transfers: Identifying deterioration can help avoid inappropriate hospital transfers, improving overall patient care.
Indicators of Deterioration
Indicators of Deterioration: Possible indicators of deterioration may include:
- Noticeable weight loss over a few months or persistent underweight.
- Poor overall health.
- Eating and drinking less
- Change in skin colour or condition.
- Pain – new or worsening pain
- Failure to return to previous health levels following an illness.
- Decreased activity and reluctance to engage.
- Increased assistance is required with walking, transferring.
- No bowel movement in 3 days
- Agitation or increased confusion.
- Persistent troublesome symptoms despite appropriate management.
- Unplanned (emergency) hospital transfers
Role of the Registered Nurse Including Assessing, Responding, and Coordinating
Role of the Registered Nurse: RNs have an obligation to assess issues that care staff team members, whānau/family report to them. They must also initiate a timely and appropriate response.
Assessing the situation: Assessment is complex. Subtle changes noted in the older person could be evidence of acute deterioration, an expected end of life process or an undisclosed social issue. Acute deterioration can be life threatening so the safest approach is to focus on confirming whether acute deterioration is present or not before considering other non-clinical causes of a changed presentation.
Responding and coordinating: New undifferentiated issues (those with unknown causes) need a diagnosis. Follow your facility policy to contact the correct health professional, e.g., general practitioner (GP), nurse practitioner (NP), or urgent care.
Vital Signs associated with Acute deterioration.
- respiratory rate: > 25 or < 10 breaths per minute
- oxygen saturation: < 93%
- temperature:
- > 37.2°C or 1°C above baseline (Sloane et al 2014) or
- > 37.2°C (twice) or > 37.8°C (once) or > 1°C over baseline (Centers for Disease Control 2023)
- < 35°C (hypothermia often indicates sepsis in ARC)
- blood pressure: systolic blood pressure < 100 mmHg
- heart rate (pulse): > 100 or < 50 beats per minute.
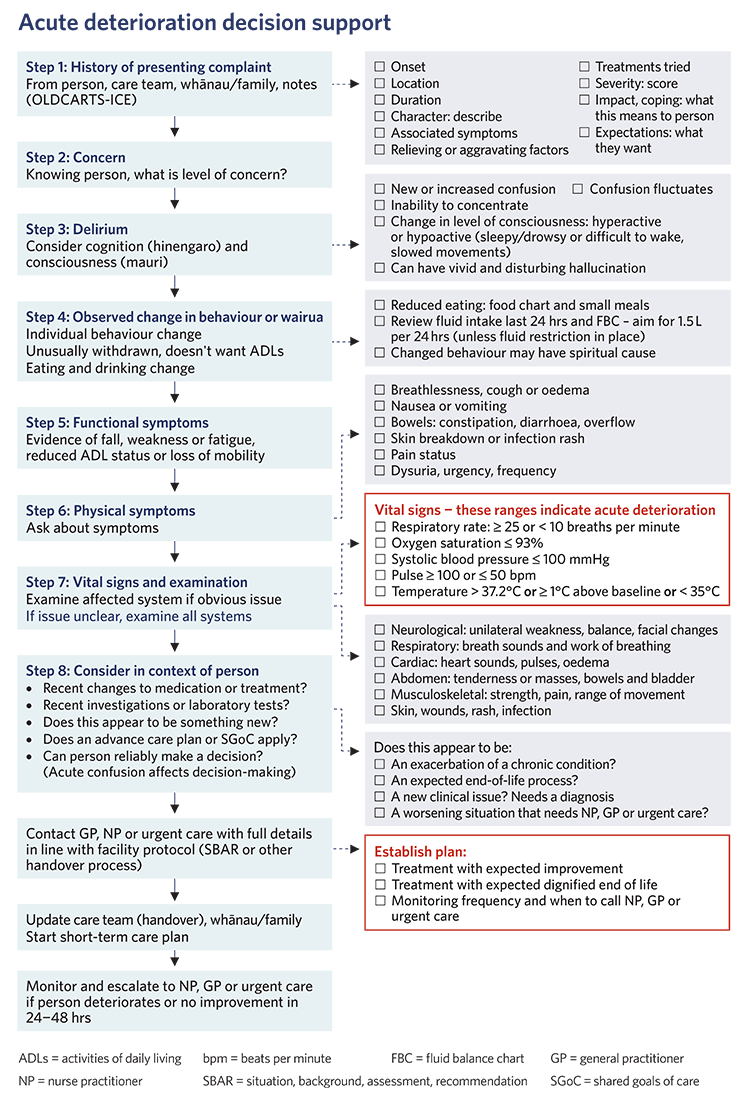
Image: Te Tāhū Hauora Health Quality & Safety Commission. 2023. Frailty care guides | Ngā aratohu maimoa hauwarea. Wellington: Te Tāhū Hauora. Reproduced under Creative Commons licence, type BY-NC-SA 4.0 https://creativecommons.org/licenses/by-nc-sa/4.0.
Communication
When someone’s health takes a sudden turn for the worse, it’s essential for healthcare professionals to respond quickly and effectively. This educational guide explains the important steps and nursing care that should be taken in these situations, with a focus on clear communication, careful planning, and thoughtful nursing care.
Communication:
- Notify Healthcare Providers: Begin by promptly communicating the situation to the Nurse Practitioner (NP), General Practitioner (GP), or the urgent care team, ensuring that critical information is relayed. They need to be aware of the situation.
- Helpful Communication Tools:
Use SBAR: Studies have shown that using communication tools like SBAR (Situation, Background, Assessment, Recommendation) can make it easier to explain what’s going on accurately (Müller et al., 2018). - Planning Care:
Creating a Short-Term Plan: Make a short-term plan that lists the things that need to be done right away and the care that needs to be provided. This helps everyone know what to do.
Working Together: Work closely with the NP or GP to figure out how often the person should be checked/ monitored, what to watch for, and when to get more help if things aren’t improving or the resident’s condition deteriorates further. - Keeping Everyone Informed: Make sure the person who is sick, their family (whānau), and anyone who is legally responsible for their healthcare knows what’s happening and what the plan is.
Sharing Information: Give all the information needed at handover so that the healthcare team understands what’s going on and how to care for the person. - Closing the Short-Term Plan: Once the person starts to improve, you can mark the short-term plan as completed.
Updating the Long-Term Plan: If the person’s overall health has changed because of this situation, update their long-term care plan accordingly.
Critical Nurse Interventions
Critical Nursing Interventions: Nursing interventions are pivotal in ensuring the quality of care that older patients and their families receive, whether aimed at recovery from an acute event or providing a safe, comfortable, and dignified end-of-life process. Key nursing interventions include:
- Spiritual Care, Comfort and Support: Offer comfort, support, and care that is focused on the person’s needs and beliefs.
- Eating and Drinking: Proper Nutrition: Make sure the person gets the right food and drinks to help them get better or stay comfortable.
- Taking Care of the Skin: Skin Health: Use good skin care practices to prevent pressure injuries and keep the person’s skin healthy.
- Moving and Positioning: Encourage the person to move and change positions to prevent them from getting too weak from staying in bed.
- Medications When Needed:
PRN Medicines: Administer medicines as prescribed following the doctor’s instructions, and make sure they are working as they should. - Monitoring and Reporting: Continuously monitor the patient’s condition and promptly update the NP/GP if the patient deteriorates, becomes distressed, or fails to show expected signs of improvement within 24–48 hours.
Responding effectively when someone’s health suddenly declines is all about working together, communicating clearly, and providing excellent care. By following these steps and giving thoughtful nursing care, healthcare professionals ensure that individuals and their families receive the best possible care, whether they’re on the road to recovery or nearing the end of their journey.






