Conversations with Liz
Best Practice for Auditing and enabling better outcomes for your residents
All rest homes and aged residential care facilities in New Zealand are certified and audited to ensure they provide safe, appropriate care for their resident and that they meet the standards set out in the Health and Disability Services (Safety) Act 2001. To ensure this quality of care is maintained the Ministry of Heath audits these facilities using designated auditing agencies audit rest homes. Each audit team includes at least one registered nurse and this audit team looks at: staff, the way residents are cared for, how the staff interact with residents, the general environment and clinical records, policies and procedures. Despite intense auditing practices, many facilities still fail to pass these regular audits. Below are some tips on how to better improve processes to simplify the auditing process and enable better outcome for your residents.
Every day is audit day!
If we have communicated our vision for our service to our staff, residents and family/whanau, trained our staff and provided the resources they need to meet the needs of residents and monitored our progress towards achieving our vision then we welcome on-site verification activity, such as inspection or examination, of a process or quality system, to ensure compliance to requirements.
So, in essence the audit verifies that you are doing what you say you will do (policies, procedures, meeting minutes, quality improvement/corrective action plans) and also meet any legislative or contractual requirements.
At the initial meeting on the first day of the audit the auditor(s) provide the service with an opportunity to discuss what improvements have been implemented since their previous audit. This is your opportunity to tell the auditors about the things you have implemented which have made a difference to staff, resident family/whanau experiences. These are quality improvement projects you want the auditors to consider awarding with a continuous improvement rating.
It is important that, as with any quality improvement projects that you can measure progress, so any data or documentation that supports the outcome of the evaluation of the success of the project is important to have at hand.
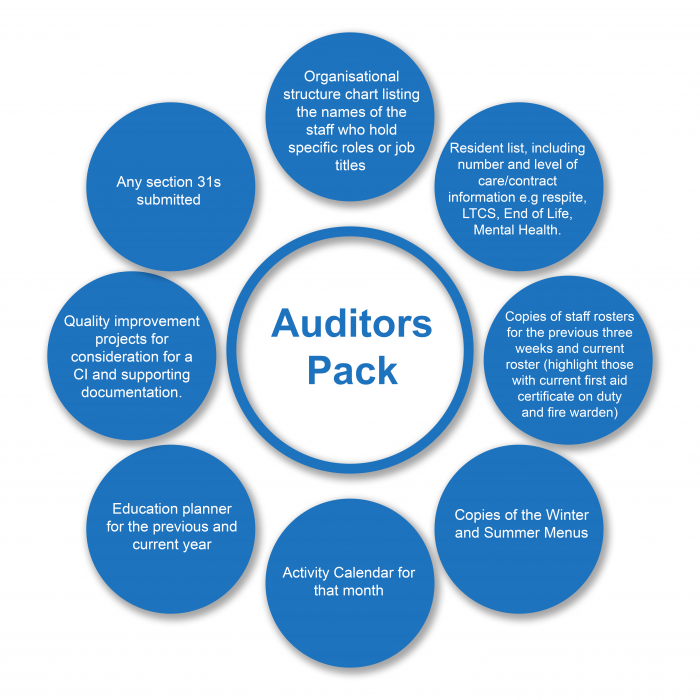
I always found that it was good to have an “auditors pack” which I could give to the auditors at the initial meeting.
These packs contained the following:
Here are some examples of the most common audit findings
Timeframes
InterRAI, long term care plans, six monthly care plan evaluations, wound care dressing changes/assessments, monitoring records (restraint, food/fluid charts, food temperatures, fridge temperatures, hot water temperatures, medication storage environmental temperature), internal audits, staff education, staff orientation, annual staff appraisals, controlled medication stock checks, trial fire evacuations, dietitian review of menu, staff/resident/quality/health and safety meetings- not occurring/completed as scheduled or within the timeframe specified or required.
Clinical documentation
- Assessment outcomes not used as a basis of care planning to link assessment to goals and interventions.
- Neurological observations not completed following a fall where the resident may have sustained a head injury.
- No evidence of RN assessment or follow up of resident concerns/changes documented in progress notes by care givers.
- Where there has been a change to resident needs/condition this has not been updated in the long-term care plan or by use of a short-term care plan which contains information and updated interventions to guide staff in the delivery of care to meet the residents’ current needs.
- Short term care plans are not evaluated by the RN at a frequency to enable monitoring of the effectiveness of the treatment/care delivery.
- Short term care plans not closed out by an RN when the issue has been resolved or transferred into the long-term care plan if it has become a chronic problem.
- Pain assessments not completed for all reports of new pain.
- Effectiveness of PRN medication administered not documented in progress notes or electronic medication charts.
- Wound care documentation does not reflect/record progress towards wound healing.
- Care plan evaluations do not describe progress of achievement towards the desired goal or outcome. Don’t just write “met’ in the evaluation section but describe how you can evidence the goal has been met. For example, “Mary had one fall in March, a review of medications was completed by the GP, and no further falls have occurred since this date. No changes are required to the current plan of care.”
- Care plans do describe triggers, distraction, de-escalation or calming techniques to manage behavioural issues. No 24 hour activity plans developed to describe the residents’ daily patterns, things/topics of interest, which staff could use to distract, minimise, or prevent challenging behaviours escalating.
- Controlled medication- pharmacy audits of controlled drug register not completed.
Register for our upcoming webinar with Auditor and Registered Nurse Liz Lear
When –Tuesday 9th November11am






