Conversations with Liz
Tips for having difficult conversations
Sharing bad news or difficult information with residents and their families can be conversations that nurses find challenging at times.
So why is it that we feel uncomfortable about having these conversations?
Nurses and health professionals report:
- Feeling apprehensive
- Questioning their competence or ability
- Feeling uncertain about what a patient may know or want to know
- Are too emotionally invested in a patient
- Find it emotionally draining
- Compromised by the environment to have private conversations
- Have a lack of time
Are you the right person to be leading the conversation with the resident/family? I ask this because if you are finding the situation stressful, this may impact on how well you engage with the resident or family. In this instance ask another more experienced nurse to lead and you can sit in as support or observer so that you can watch and learn.

Using the SPIKES model for breaking bad news can help you plan and keep your thoughts focused.
S- Setting
Where will this conversation take place, when and at what time? Ideally you want a quiet environment with no interruptions. Let others know what is happening so that you are not disturbed.
Read the residents notes and prepare what you need to say.
P- Peception and I- Invitation
Before you share any information, find out what the person already knows and understands. By doing this, you will be able to judge what you need to say. Start with an opening question. For example,
‘Tell me what you know of your mothers health?
‘What have you been told so far?’
To demonstrate you are listening to the resident or family member, you might repeat what you have heard and check that you have got this right. You might say something like;
“Just to check that I have understood you, you have been told that your conditions is getting worse, and that it will continue to deteriorate and you will not get better. Have I got this, right?’
Do not be afraid of silence. Silence allows people to process what they have heard and think of how they will respond.
K-Knowledge
Up to this point you have been asking questions to gather information about what the person knows and what they might want to know. You are now in a position to start sharing difficult news.
Summarise what has happened so far. You might want to provide examples of how the patient’s condition has progressed or deteriorated.
Before you proceed to communicate the difficult information, give some warning. An example of this might be,
“The news isn’t good, I am afraid.”
Give information in small amounts. People on the receiving end of difficult information or bad news will only retain a small amount of information. They need time to process the information. Their emotions will be heightened
E-Emotions and Empathy
When having difficult conversations where you convey bad news to someone, it will induce some emotional reaction. If they cry, let them cry. Acknowledge the emotion with an empathic response.
“I sense that this is very difficult for you to hear.’
You can show empathy in your posture and the way you interact with someone. Sitting with someone (if you can) will also convey you have time for them at that moment. Listening and showing you are listening to someone will have meaning, as will noticing their distress.
S- Summary/Support
Draw the conversation to a close. Is there anything that you need explain again?
- Can you offer any information about what may happen next?
- Signpost them to some supportive services?
- Explain your approach to care moving forwards. e.g. symptom control
Although it is never easy to have these types of conversations having a plan of action provides structure for this difficult discussion and helps support all involved.
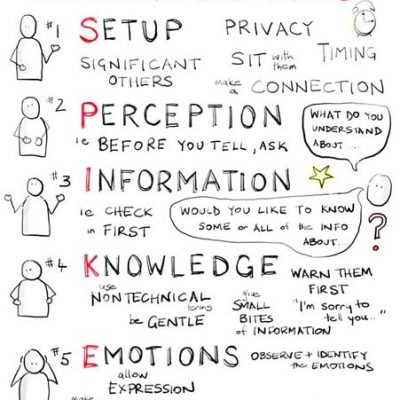
Image credit: SPIKES: A Strategy for Delivering Bad News (utah.edu)
Register for our upcoming webinar with Auditor and Registered Nurse Liz Lear
Free handover report template for all those who register and attend the webinar
When – Wednesday 4th August 11am






